UNODC supports Central Asian countries in piloting quality assurance mechanisms/tools for drug use disorder treatment
Background
In 2019, four Central Asian countries – Kazakhstan, Kyrgyzstan, Tajikistan and Uzbekistan – piloted the implementation of UNODC's quality assurance mechanisms/tools for the treatment of drug use disorders.
The event was held within the framework of UNODC's global project GLOJ71: "Treatment of Drug Dependence and Its Health Consequences: Tritnet II" with the financial support of the U.S. Department of State's Bureau of Narcotics and Law Enforcement (INL).
Following the training of drug use disorder treatment professionals from each country , teams of trained evaluators selected standards, criteria and methods for assessing service quality control from UNODC's toolkit for piloting. Countries focused on areas that they considered important in their country or that needed improvement. The selected standards were piloted for 10 drug dependence treatment services in 13 centers.
The report, prepared by UNODC's international consultant, Ms. Annette Dale-Perera, presents the comparative results of four Central Asian countries that participated in the piloting of UNODC's quality control tools.
Outcomes
All countries have shown significant commitment to piloting quality assurance tools for drug use disorder treatment services based on UNODC's Quality Assurance Framework. The countries and services involved are to be commended for their diligence and commitment to the quality recommended by UNODC.
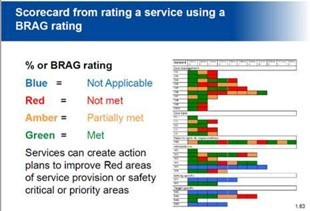
Overall, the results of the evaluation showed the following:
- Most services meet many criteria, including 65% of the general criteria chosen by all services and 76% of all criteria.
- Central Asian countries have the necessary conditions for the functioning of services, including national regulations, assessment procedures, patient and staff registration systems.
Key trends in service compliance:
- For most of the criteria of the "Main Management" standards, a score of "compliant" was obtained. However, some improvement was required (for two or more services) according to the following criteria: revision of service plans; staff training; clinical management mechanisms; Patient consent. Moreover, for Key Performance Indicators (KPIs), improvement is required on the occupancy waiting list for patients completing treatment and their follow-up care.
- The key factors in the Basic Care standards were that 21 criteria were rated "compliant" (57%) and 16 (43%) criteria were rated "non-compliant" or "partially compliant". Improvement was required (in two or more services) across all criteria, in particular treatment planning in one country and review/revision of treatment plans (in three out of four countries).
- A key factor in the Patients' Rights standards was that patients generally reported being treated with respect. However, there was room for improvement in terms of "patients feel involved in the assessment" and "treatment planning" criteria. Most countries could also improve patient participation in quality assurance and service design.
- In terms of "Intervention" standards, some countries met certain criteria for the availability of intervention protocols, in particular opioid pharmacological interventions. However, in some countries, physical and mental health assessment protocols need to be improved; protocols for psychosocial interventions; protocols of pharmacological interventions for detoxification of sedatives; symptomatic prescription and treatment of combined consumption of surfactants. There was also no evidence provided as to whether the protocols were approved and used in the services.
- With regard to the Treatment Setting/Facility Standards, three of the four countries required improvement of outreach protocols.
- With regard to the "Task Force" standards, three countries required protocols for dealing with parents who use drugs, including women.
Recommendations
Following the success of this pilot project, it is recommended that the project be reviewed and that a regional quality assurance mechanism be initiated. This may include:
- The standards and criteria of the quality assurance framework should be revised and aligned with the latest International Standards for the Treatment of Drug Use Disorders (WHO/UNODC, 2020) and the UNODC Quality Assurance Toolkit, 2020 version.
- A harmonized set of "Consensus Standards" and criteria (including KPIs) could be developed for the region to promote the exchange of best practices, benchmarking and peer auditing. If necessary, countries may also implement "extra" criteria in addition to the above.
- In the second phase of the implementation of the quality assurance mechanism, the criteria for evaluating the "Intervention" standards should include information on whether protocols are in place within the services, as well as whether documentation is available. This will be an indicator of whether staff are adhering to evidence-based, agreed practices.
- Ideally, the implementation of a quality assurance framework should include harmonized methodologies, including patient surveys, and methods for reporting on them, which can be strengthened as part of future training and implementation of a quality and accuracy assurance mechanism.
A second phase of training and technical support provided by UNODC to consolidate the quality assurance framework to scale up implementation was also recommended. This phase will begin in October 2020.
